Outlook for Obamacare
The Affordable Care Act of 2010 was a milestone in the long fight for health care reform in the U.S. But despite President Obama’s reelection, it is far from clear whether it will deliver on its promise. A close examination of the question of implementation.

A patient at Scripps Urgent Care Clinic, San Diego, March 1, 2011. Peggy Peattie/San Diego Union-Tribune/ZUMA Press/Corbis
As we approach the thirty-fifth anniversary of the Alma Ata Declaration calling for universal access to essential health services, stakeholders around the world are making a renewed commitment to universal health coverage. Margaret Chan, director general of the World Health Organization (WHO), recently declared that universal health coverage is the best way to cement the gains made in global health. It is, she said, “the ultimate expression of fairness [and] the anchor for the work of WHO as we move forward.” The Lancet medical journal devoted its entire September 2012 issue to universal health coverage, highlighting the public health benefits of improving access to care as well as the positive economic and political implications. Researchers from the Council on Foreign Relations’ Global Health program recently described universal health coverage as “the new global health agenda.” Other recent efforts—such as the work of the Joint Action and Learning Initiative on National and Global Responsibilities for Health—seek to develop a post-Millennium Development Goal framework rooted in the right to health and aimed at securing universal health coverage for all.
Universal health coverage—and its promise of access to quality care—is increasingly cast as a global social norm and moral imperative. Access to affordable health care ranks among the tenets of the right to health, which is reflected in international instruments dating back to 1946 including the United Nations Declaration on Human Rights and the WHO Constitution, among others.
Many countries have long embraced the concept of universal health coverage, and the number of countries launching universal coverage programs continues to rise. The world’s twenty-five wealthiest nations (with the exception of the United States) have already adopted universal health coverage as have countries as diverse as Brazil, Ghana, Kuwait, Mexico, Rwanda, Saudi Arabia, and Thailand. Emerging-market countries such as China and India have signaled their intention to expand access to coverage. And others are following suit: nearly one hundred countries have begun to study the feasibility of publicly financed health programs. And, in response to a 2010 WHO report on making universal coverage a reality, more than sixty middle- and low-income countries have requested technical assistance to further their goal of universal health coverage.
Despite the global momentum for universal health coverage elsewhere and numerous attempts to implement it domestically, the United States has been unable to broadly expand access to coverage. This is largely because health care has long been a contentious political issue in the United States. Indeed, although a number of presidents and congressional leaders—including Senator Claude Pepper as early as 1943, Senator Ted Kennedy beginning in the 1960s and throughout his career, and President Bill Clinton as recently as 1993—have attempted to achieve universal coverage, these efforts ultimately failed in the face of ardent opposition from powerful special interests—physicians, the insurance industry, and other stakeholders. Without political support for broader reform, policymakers were able to make only incremental changes to health insurance coverage in the United States.
But, building on this history of incremental change, President Barack Obama signed landmark health reform legislation on March 23, 2010, thus securing a legislative achievement that had eluded many of his predecessors. The legislation—the Patient Protection and Affordable Care Act of 2010 (ACA)—establishes a pathway for coverage of nearly all Americans, and puts the United States’ health system closer than ever before to its industrialized peers. Before the 65th World Health Assembly in May, the U.S. secretary of Health and Human Services described the ACA as the country’s “most significant step towards universal health coverage in nearly fifty years.”
The ACA has the potential to transform the accessibility, adequacy, and affordability of health care in the United States and to add to the growing momentum for universal health coverage around the world. Yet, because the ACA adopts America’s existing federalist framework—requiring cooperation between state and federal governments—much must be done to prepare for 2014, when the ACA’s most significant reforms are due to take effect. States and the federal government must make changes to implement the ACA. There will be repercussions if state and federal regulators fail to make these changes, thereby threatening the ACA’s promise of access to coverage in the United States.
Higher Costs, Poorer Outcomes
To understand the ACA, one must first understand the challenges of the United States’ complex and costly health care system. The United States is home to the most costly health care system in the world. In 2010, over 17 percent of the nation’s total economic activity (and $8,402 per person) was spent on health care, with health care spending expected to expand to nearly one-fifth of GDP by 2020. High health care costs have broad implications for federal spending and the economy. For example, the cost of public health care programs is increasingly financially unsustainable, as the United States government is forced to spend more and more each year to provide health coverage for elderly and low-income Americans. High health care costs also affect the private sector: some argue that the costs of employer-sponsored private insurance inhibit the competitiveness of American businesses abroad.
Despite high costs, Americans have poorer health outcomes than counterparts in other industrialized nations. The United States frequently finds itself ranked among middle- and low-income countries on indicators such as infant mortality and life expectancy. These health outcomes are likely to be exacerbated as older generations retire and the prevalence of chronic diseases continues to rise.
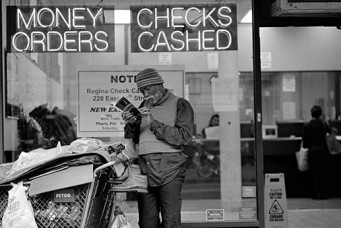
Poor health outcomes are also linked to the fact that 15.7 percent of Americans—nearly 49 million people—are uninsured. The majority of Americans—197.3 million—purchase private health coverage through their employer. But, because many cannot afford private health insurance, their employer does not offer coverage, or they do not have access to affordable care that meets their health needs, high levels of uninsured persist. This is true even with public programs such as Medicare, Medicaid, and the Children’s Health Insurance Program (CHIP), which cover an additional 99.5 million individuals.
These programs, while critical, have strict eligibility requirements and are not available to all Americans. Medicare, for example, provides coverage for individuals age 65 and older and individuals with certain disabilities; Medicaid primarily provides coverage for a different population—low-income women and children—but with eligibility rules that vary by state. Other public programs exist at the state level: for example, thirty-four states operate a high risk pool as a “last resort” for individuals with preexisting conditions. Even though these are public programs, enrollment is not without costs. Most Americans pay premiums towards their Medicare coverage and face significant out-of-pocket costs for prescription drug coverage and supplemental health insurance. And even coverage in a high risk pool has premiums that can be unaffordable for individuals with preexisting conditions.
In addition to high health costs and a high uninsured rate, the United States operates with a highly complex, federalist regulatory system that often requires cooperation between state and federal governments. Private health insurance is regulated by the federal and state governments, depending on where a consumer lives and works. This dual system of regulation is complicated and can lead to fragmented rules for insurers and confusion for consumers who do not know which rules apply to their coverage.
One example of this complex federalist regulatory system is seen in the regulation of “self-funded plans” (group health plans purchased by employers). As noted above, most Americans purchase private health coverage through their employer; among those that do, most are enrolled in self-funded plans. Under a federal law passed in 1974, these plans are exempt from many state regulatory requirements. While states regulate the insurer that sells the group coverage, state regulators do not have as much authority over these plans as they do over coverage for individuals and small businesses. Thus, the regulation of self-funded plans—and coverage for millions of Americans—is largely left to the federal government.
Because private health insurance purchased by individuals and small businesses has historically been regulated by the individual states, rules and consumer protections in these markets vary significantly across the country. For example, a consumer buying individual health insurance in one state, such as New York, may have different consumer protections than a consumer in another state, such as Maryland.
At the same time, the federal government increasingly sets standards for private health insurance by passing new laws, such as the ACA. Yet, because states remain the primary regulators of health insurance, the federal government is largely dependent on states to adopt and enforce new standards, particularly in the individual and small group markets. Although the federal government retains the ultimate authority to enforce federal law, federal officials do so only if a state informs the federal government that it is not enforcing the law or if the federal government finds that a state has failed to “substantially enforce” the law. This complicated “federalist” approach requires states to not only enforce their own laws and requirements but also gives states significant flexibility in how (and whether) they enforce minimum federal standards, with federal enforcement as a “back-up plan.”
Like private health insurance, public programs—such as Medicare, Medicaid, and CHIP—are also regulated at both the federal and state level. Medicare, a program that covers older and disabled Americans, is regulated almost entirely at the federal level. In contrast, Medicaid and CHIP are regulated by the federal and state governments and—like private health insurance—rules vary dramatically from state to state. For example, under Medicaid, the federal government establishes minimum standards for whom and what must be covered, and provides significant funds to states to establish and administer Medicaid coverage. Thus, states play a critical role in setting rules for Medicaid eligibility, benefits, and enrollment.
While public programs exist to protect the old, the sick, and the very poor, there are few options for lower-income Americans—such as the working poor—who often do not have access to employer-sponsored coverage. While many attempts have been made to try to secure coverage for this segment of the population, none has been successful. That is, until President Obama signed the ACA, which has been dubbed “Obamacare” by proponents and detractors alike.
The ACA has the potential to change health care in the United States and add to the growing momentum for universal health coverage around the world. Through significant changes to the regulation of private health insurance, federal subsidies for low-income workers to purchase private health insurance, a mandate that requires individuals to secure and maintain health coverage, and the expansion of the Medicaid program, an estimated thirty-two million Americans are expected to be newly insured once the ACA is fully implemented. Of these, 16 million will be eligible for coverage through the Medicaid program. With these increases in coverage, the rate of insured citizens in the United States is expected to increase from 83 percent to 94 percent. (The ACA would not cover about 23 million nonelderly residents, including about one-third of whom would be unauthorized immigrants.)
These gains, however, have been highly controversial and critics have been vocal in decrying the ACA. Opposition to the ACA has become a rallying cry for the Republican Party since the law was passed in 2010. The ACA is also opposed by a new grassroots political movement known as the Tea Party, which is largely allied with the broader Republican Party and helped overturn a Democratic Party majority in the United States House of Representatives in the country’s 2010 congressional elections. With the two chambers of Congress now divided between a Republican-controlled House of Representatives and a Democratic-controlled Senate, partisanship clashes between the two chambers—and consequential legislative gridlock—have become commonplace and public approval of Congress is at record lows.
Republican critics largely argue that the ACA raises health care costs, hurts the economy, and represents a “government takeover” of the health care system. Leaders in both the Republican Party and the Tea Party movement—as well as Republican Party presidential candidate Mitt Romney—pledged to “repeal and replace” the ACA. In fact, the House of Representatives has already voted—repeatedly—to repeal all or part of the ACA. These votes were symbolic because the Democratic-controlled Senate was unlikely to approve repeal legislation, and President Obama threatened to use his veto power should such legislation pass both chambers. Not surprisingly, Obamacare became a contentious issue in the 2012 U.S. presidential election contest between Obama and Romney, underscoring the ACA’s vulnerability to political battles.
In any case, gains in coverage will not be realized immediately because the ACA is designed to be implemented in phases. In fact, many of the law’s most significant reforms will not be fully implemented until 2014, with additional changes beginning as late as 2017. In its first phase in 2010, the ACA required private insurers in the individual and small group markets to make critical changes to their insurance policies and practices by, for example, spending more on medical care than on administrative costs and profit. The law also required increased transparency through meaningful appeal processes and federal funding for consumer assistance and rate review programs.
In 2014, the ACA ushers in its most significant reforms, particularly for individuals and small businesses. The ACA prohibits insurers from denying coverage to any American including those with preexisting conditions; restricts the rates that insurers can charge for coverage; requires insurers to cover a minimum set of services known as “essential health benefits”; and limits the amount of out-of-pocket costs that consumers can be forced to pay for coverage. Because these requirements differ from current insurance rules, states that choose to adopt and enforce the ACA will likely have to pass new legislation or issue new regulations.
Also in 2014, the ACA requires the establishment of health insurance “exchanges” in each state. Exchanges are organized marketplaces designed to help individuals and small businesses shop for private health coverage and make easy comparisons among plans that meet minimum quality standards. Consistent with the federalist framework for private health insurance, exchanges can be state-based (designed and fully administered by the state), federally facilitated (designed and fully administered by the federal government), or operated through a partnership (jointly designed and administered by the state and federal government).
At the same time, the ACA introduces new requirements for individuals to obtain coverage or face a tax penalty. The use of this “individual mandate” contrasts sharply with how most nations have adopted universal health coverage. While most countries view the provision of health care as the government’s responsibility, the ACA reflects the United States’ staunch commitment to individual responsibility by placing the burden of coverage on individuals through purchase from private insurers.
The individual mandate was the subject of a Supreme Court decision in June 2012 that largely upheld the ACA as constitutional. The only area where the Supreme Court limited the ACA was with respect to Medicaid expansion. As written, the ACA required state Medicaid programs to expand coverage to all individuals with incomes under 133 percent of the federal poverty level or risk losing funding for their existing Medicaid program. The costs of covering this new population would be fully funded by the federal government through 2016 with the federal government paying for 90 percent of costs thereafter. The Supreme Court found this requirement to be unconstitutional, a decision which gives states the choice of whether to expand Medicaid coverage to this new population or not. Like the reforms for private health insurance, implementing this requirement will likely necessitate a change to existing law through new legislation or regulations for most states.
Although a step forward for millions of uninsured Americans, even ACA supporters recognize that the law builds upon an existing, highly fragmented regulatory system. Instead of introducing dramatic change by, for example, allowing Americans to purchase coverage directly from the government, or establishing a “single-payer system” (a common public pool funded by employers, employees as well as the government), the ACA largely maintains the status quo: a patchwork system of private and public insurance regulated by the federal and state governments and delivered through private organizations.
And there is no shortage of critics who claim that the ACA did not go far enough. Many have criticized the ACA for not doing enough to address the high cost of health care and instead focusing largely on how health care is delivered. Others argue that the ACA will not affect coverage for millions of Americans because the law did little to change the regulation of self-funded plans, which account for the majority of the private health insurance market in the United States and are largely unaffected by the ACA’s most significant reforms. Still others sound the alarm that the ACA will only exacerbate the country’s shortage of health care workers and do little to address the poverty that many of the newly insured face. Further reforms are likely needed to address these issues.
The Critical Role of the States
Even though President Obama signed the ACA back in 2010, key questions persist about how it will be implemented. The federal government has already issued important regulations on new private health insurance rules, which went into effect in 2010, as well as minimum standards for health insurance exchanges, and many other ACA reforms. However, federal regulators have yet to issue regulations clarifying the reforms that go into effect in 2014, how to define a package of “essential health benefits” that insurers will have to cover, or what a federally facilitated exchange will look like. Because these regulations will further define the rules by which these critical reforms will operate, federal regulators will continue to play a significant role in ACA implementation.
Yet, in the midst of uncertainty about federal requirements, states must make significant decisions that will directly affect whether the ACA fulfills its promise to expand coverage to thirty-two million Americans. For one, states can choose to adopt and enforce the ACA’s new consumer protections or allow the federal government to do so. States can also choose to establish state-based exchanges, partnership exchanges, or federally facilitated exchanges. And, following the Supreme Court’s decision, states can choose whether or not to expand their Medicaid programs.
To date, states have adopted a variety of approaches to ACA implementation, with some embracing the law and others vowing not to implement any components. The politics of the ACA notwithstanding, most state officials have approached health reform pragmatically and have taken, perhaps, more steps to implement the ACA than conventional wisdom suggests. What follows is a snapshot of state efforts to implement the ACA’s private health insurance reforms, health insurance exchanges, and Medicaid expansion.
Private Health Insurance Reforms. Although most reforms will not take effect until 2014, a set of new consumer protections—referred to as the “early market reforms”—went into effect in September 2010. These provisions, which are fairly popular, include allowing a child to remain on a parent’s health insurance plan until the age of 26 and requiring insurers to cover certain preventive services without out-of-pocket costs for consumers, among others.
In a study on how states have implemented these new requirements, researchers from Georgetown University’s Center on Health Insurance Reforms found that the vast majority of states and the District of Columbia took new action to require or promote compliance with these protections. Indeed, forty-nine states and the District of Columbia passed new legislation, issued a new regulation, issued new sub-regulatory guidance, or are actively reviewing insurer policy forms for compliance with these protections. These findings are supported by case studies of individual states—and a summary of actions in ten states—where regulators reported few, if any, complaints regarding the early market reforms.
States have also amended or passed new laws in response to the ACA’s requirement that states review rate increases. This is in part because states that fail to review premium increases face federal enforcement of these rules. State regulators reported that the threat of dual regulation sufficiently incentivized the state to adopt the ACA’s requirements. And a few states—such as Connecticut, Maine, and Maryland—have even begun making changes that will go into effect in 2014. These states will, for example, enforce the ACA’s requirements that insurers cover “essential health benefits” and not charge different premiums based on gender or how healthy someone is.
Even in states where the ACA is extremely unpopular, the threat of dual regulation—by both the federal and state government—has resulted in at least some implementation of the ACA. The year 2013 could be a critical one for state policymakers to decide whether to adopt and enforce the ACA’s requirements or allow the federal government to do so.
Exchanges. The ACA requires a health insurance exchange to be established in every state. An exchange is an online marketplace for individuals and small businesses to purchase health insurance and is designed to increase transparency and competition. Exchanges are not a new concept in the United States and many states have established or considered establishing exchanges prior to the ACA. States can choose to develop a state-based exchange, allow the federal government to establish a federally facilitated exchange, or partner with the federal government to operate a partnership exchange.
State exchange implementation under the ACA has been decidedly mixed. Researchers from George Washington University report that only eleven states and the District of Columbia have passed new legislation to establish an exchange while governors in two additional states—New York and Rhode Island—signed executive orders to establish an exchange for their residents. Since this report, the governor of Kentucky also signed an executive order to establish an exchange.
Even though few states have obtained legal authority to establish an exchange, most have used federal funding for exchange planning and development. To date, all but one state received a $1 million exchange planning grant with most states receiving additional funds to develop and operationalize an exchange. To date, the United States has contributed an estimated $1.78 billion towards exchange development.
Without regulations regarding what a federally facilitated exchange might look like, many states face uncertainty in making exchange decisions. This is important because states must select an exchange framework by November 16, 2012. This is the due date for states to complete a “blueprint” that outlines the state’s ability to make an exchange a reality. All eyes will be on the states during their 2013 legislative sessions to see if they establish their own exchanges or set rules on how an exchange will operate.
Medicaid. Although rendered optional by the Supreme Court’s decision, many states have already begun preparations for Medicaid expansion under the ACA. According to research from the Kaiser Commission on Medicaid and the Uninsured, forty-eight states and the District of Columbia had taken steps on at least one of five Medicaid-related actions as of May 2012. Eight states have already expanded their Medicaid programs to cover individuals with incomes up to 133 percent of the federal poverty level ahead of 2014, and twenty-eight states and the District of Columbia have submitted or approved plans to upgrade their Medicaid eligibility systems.
Notwithstanding these efforts, some states have indicated that they will not participate in Medicaid expansion in 2014. Because Medicaid is expected to cover half of all newly insured Americans in 2014, state expansion will be critical in realizing the ACA’s promise of near-universal coverage. Unfortunately, it remains to be seen whether populous states with high rates of uninsured—such as Florida and Texas—will expand their Medicaid programs or not. If these two states, alone, do not expand their Medicaid programs, it will reduce the number of Americans covered by the ACA by about three million people and could have a significant impact on access to coverage.
Cause for Celebration?
Domestically, there is much uncertainty as to whether the ACA will be able to deliver on its promise of near-universal health coverage. Because states play a prominent role in the United States’ complex federalist regulatory scheme, state decision-makers have the opportunity to shape how the ACA’s reforms will be enforced, how the insurance exchanges will be run, and whether Medicaid coverage is delivered as promised. If political opposition to the ACA continues and states refuse to adopt and enforce the ACA’s requirements, some of the law’s consumer protections and its promises of access to affordable, adequate, and accountable coverage could be at risk.
Despite this uncertainty at the domestic level, the law brings the United States one step closer to the global ethic of universal health coverage. While much of the international community has been confounded by the political furor over universal health coverage in the United States, the ACA represents a remarkable shift in the way that private insurance is regulated by taking pains to enable every American—including the sick—to access coverage.
While imperfect in many ways, the ACA could generate additional momentum for improvements in universal access to coverage around the world as other countries look to the United States because of its prominent role in striving to improve global health. The law could also lend additional credibility to the United States in its leadership role at WHO and in the global health arena where it has often supported universal health coverage policies while failing to pursue these reforms on its own soil. Finally, with the aim of securing near universal health coverage for its residents, the ACA helps align American domestic policy with long-standing foreign policy and support for universal health coverage, particularly in developing countries.
What’s next for the universal health coverage movement? As more and more people obtain coverage, attention will increasingly turn to the quality and cost-effectiveness of coverage. The need to ensure cost-effective, quality care has never been more important, particularly in developing countries which increasingly face the burden of non-communicable diseases like heart disease, cancer, diabetes and respiratory illness in addition to infectious diseases and malnutrition. This epidemiological transition—from infectious diseases to chronic diseases—will have a significant impact on health care systems around the world. Indeed, by 2020, seven out of every ten deaths in developing countries are expected to result from chronic diseases. These rapidly evolving needs suggest that quality, cost-effective coverage will be important as ever in protecting the public’s health, both in the United States and around the world.
Yet, because of the complicated political, cultural, and economic contexts within which countries operate, no single program can serve as an ideal health care model for the world. Rather, policymakers must consider how existing models for health care financing can be adapted to meet the needs of the population amidst their own social and political contexts. In this respect, the American experience with the ACA has the potential to contribute to a body of collective insights and joint learning on universal health care. As analysis of ACA implementation continues, other countries may draw upon the challenges faced in the United States in pursuing universal health care initiatives.
One thing is certain: health reform will be an ongoing process in the United States and around the world. Although the ACA will not fundamentally alter the way health care is provided in the United States and does little to address a looming health care worker shortage and the high cost of care, Obamacare has already improved access to coverage for millions of Americans and should be celebrated by proponents of universal health coverage domestically and abroad.
Katie Keith is an assistant research professor at Georgetown University’s Center on Health Insurance Reforms. Her work has been featured in the Washington Post, Kaiser Health News, Modern Healthcare, and other publications.
Tanya Baytor is the Global Health Law LL.M. Program Director and an adjunct professor of law at the O’Neill Institute for National and Global Health Law at Georgetown University Law Center. She specializes in global health law and has worked on projects with the World Health Organization, the World Bank, and the InterAmerican Heart Foundation, among other organizations.